This blog post reports on work-in-progress within the DfG course! The post is written by group 2B dealing with Kela and the Ministry of Social Affairs and health’s brief on continuity of care as a New Kela reimbursement model. The group includes Bhairavi Balasubramanian and Sofia Correia from the master’s programme in Collaborative and Industrial Design and David Bertl and Tuomas Laakkonen from the master’s programme in Creative sustainability.
Written by: Bhairavi Balasubramanian
On the previous episode of the Continuity of Care series;
In our last blog post, we covered topics such as the bowtie of possibilities, the situation of the current Finnish healthcare system, and where we plan to intervene. Before you continue reading this, I would highly recommend that you visit the previous blog to get an understanding of this blog and the following ones.
You can read the previous blog of this series here
Now, let us see how we have proceeded from then to now.
Experts always know it all!

Activity with Experts© Creative Commons CC by 4.0. 2024. Bhairavi Balasubramanian, Sofia Correia, David Bertl and Tuomas Laakkonen. Design for Government. Aalto University.
After concluding that we wanted to focus on the needs and the role of general practitioners across the four doors, we decided to contact general practitioners and other experts in the industry. This was aimed not only at understanding the nuances of the healthcare system but also at gaining insight from a general practitioner’s perspective. After interviewing four experts from the industry with different sub-areas of expertise and supporting it alongside desk research, we discovered some key findings.
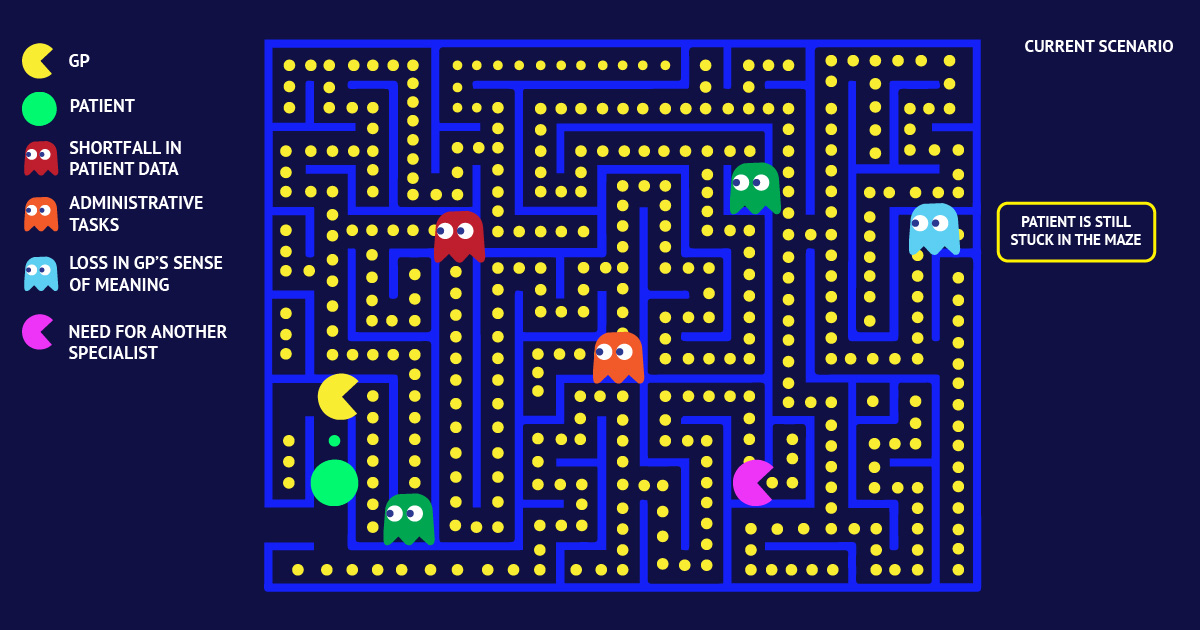
The Pacman of healthcare.
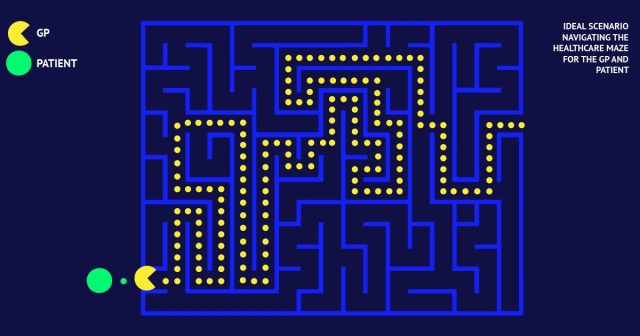
Ideal Situation: The Pacman of healthcare (Inspired by Pacman) © Creative Commons CC by 4.0. 2024. Bhairavi Balasubramanian, Sofia Correia, David Bertl and Tuomas Laakkonen. Design for Government. Aalto University.
This is the maze of healthcare. The general practitioner plays a key role in managing the patient’s journey in this maze of healthcare. A successful journey occurs when the GP (General Practitioner) comprehends the patient’s needs and guides them through the maze without ambiguity or confusion. Consequently, the patient achieves the best possible outcome, leaving the GP aware of their results and satisfied with their work.

Current Situation: The Pacman of health care (Inspired by Pacman) © Creative Commons CC by 4.0 .2024. Bhairavi Balasubramanian, Sofia Correia, David Bertl and Tuomas Laakkonen. Design for Government. Aalto University.
Currently, due to a lack of patient history and insufficient data, along with challenges such as infrequent encounters with the same patient and organizational issues, the patient does not receive the best possible outcome. Despite these obstacles, the GP continues to strive for improvement within a flawed system Regarding health and diseases, the GP endeavors to address most illnesses unless they determine that the issue requires intervention from a specialist.
This highlights the extensive responsibilities that a GP manages both administratively and medically within this complex system, despite not always achieving desired outcomes. It also highlights the indispensable nature of their role within the healthcare system.
Now that I have walked you through the importance of a General Practitioner in the healthcare system, and the number of duties they must perform, this also connects to the immense work pressure and poor working conditions for them which in turn, makes them either further specialize or leave the public sector.
This brings me to my next insight,
The Exodus cycle of general practitioners.
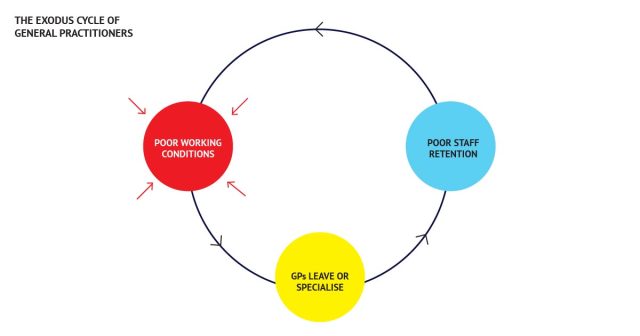
The Exodus cycle of general practitioners © Creative Commons CC by 4.0. 2024. Bhairavi Balasubramanian, Sofia Correia, David Bertl and Tuomas Laakkonen. Design for Government. Aalto University.
The diagram above explains a particularly vicious cycle within the healthcare industry concerning General Practitioners in the public sector. The heavy workload faced by GPs in the public sector, along with other factors (which we will explore shortly), contributes to poor working conditions for them. This situation often leads them to pursue further specialization in specific areas of care, where post-specialization opportunities are broader and offer more flexibility in terms of sectors and job types. Alternatively, it may compel them to exit the public sector entirely, opting instead to become occupational physicians or private practitioners. Consequently, this exacerbates the issue of scarce staff retention among GPs in the public sector, resulting in fewer doctors, increased work pressure, and significant costs incurred by public healthcare organizations due to the need for frequent recruitment and training of new personnel. This also leads to a lack of continuity in patient care due to GPs constantly changing.
This led us to focus on the red circle representing the poor working conditions of GPs, enabling us to collect data and gain an understanding of the specific conditions and how they are caused.
Zooming into poor working conditions
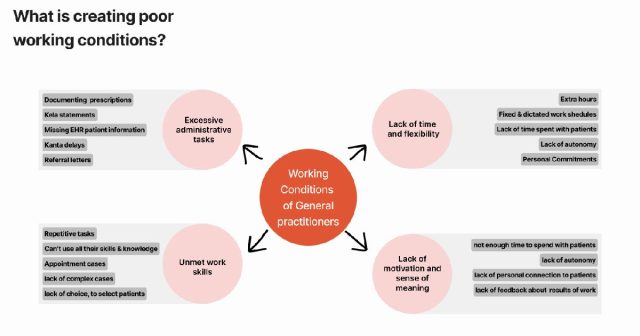
What is causing poor working conditions and why? This is something our experts helped us answer and understand. Based on their experiences, we defined four major problem areas, as seen above, and what is causing them. Some very interesting insights and quotes were highlighted under each category. For example, we interviewed an occupational physician who is currently also working as a researcher at Kela. They spoke about how they previously worked as a public GP and worked extra time doing administrative tasks such as renewing prescriptions, writing statements for Kela, writing referrals, and more tasks like these. He handled this workload earlier, but after starting a family, he had other duties like picking up his kids from school and taking them to hobby classes. This prompted him to switch to occupational healthcare since it offers a lighter workload and allows the doctor to manage his own schedule based on his availability and flexibility
Many insightful stories as such were collected and helped us understand the poor working conditions in detail.
In wrapping up my experience, the past few days have been a rollercoaster of significant thoughts and insights condensed into bite-sized diagrams and short sentences. It has been about finding clarity within us and conveying it effectively to others. Understanding the Finnish healthcare system, coming from a different healthcare background back home has been complex yet incredibly rewarding. In a funny sense, I would have never imagined myself to be contacting doctors in Finland a year ago, but here I am, surprisingly myself every day.
But what next?
Now that we have understood the Exodus cycle and what starts it, where can we step in and break it? and how?
To know that, keep following this space!
The DfG course runs for 14 weeks each spring – the 2024 course has now started and runs from 26 Feb to 29 May. It’s an advanced studio course in which students work in multidisciplinary teams to address project briefs commissioned by governmental ministries in Finland. The course proceeds through the spring as a series of teaching modules in which various research and design methods are applied to address the project briefs. Blog posts are written by student groups, in which they share news, experiences and insights from within the course activities and their project development. More information here about the DfG 2024 project briefs. Hold the date for the public finale on Wednesday 29 May!