This blog post reports on work-in-progress within the DfG course! The post is written by group 2C dealing with the Ministry of Social Affairs and Health’s brief on Continuity of Care as a new Kela reimbursement.
The group includes Sofia Pascolo and Devayani Mohanraj from the master’s programme in Creative Sustainability, Heidi Mäkitalo from the master’s programme in Computer, Communication, and Information Sciences program (Human-Computer Interaction Major), and Robert Hartmann from the master’s programme in Collaborative and Industrial Design.
Written by: Devayani Mohanraj
Up until now, we have been trying to truly understand the Finnish healthcare system and its various facets. Our group is focusing on the patient’s perspective, and we discussed many insights, opportunities, and ideas to improve continuity of care for patients. The main long-term opportunity that we identified was that continuity of care can improve the efficiency of the healthcare system by reducing consultation times, improving diagnosis, reducing costs, and enhance overall service and satisfaction for everyone. However, in the short term, we would need to focus on the heavy users, such as the chronically ill and elderly, and providing continuity of care to them would create larger benefits for the system.
Defining a Vision
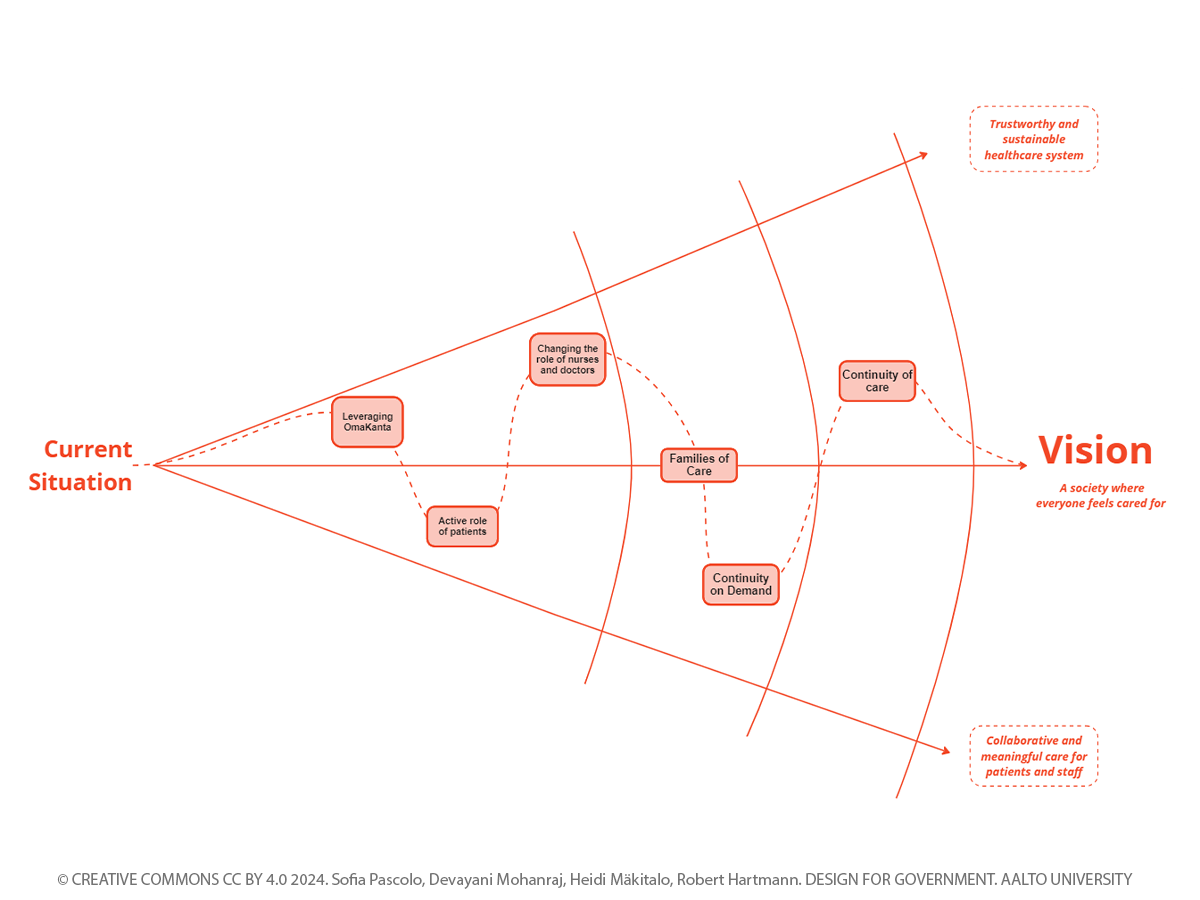
How does vision dictate large-scale change? The vision is the larger picture, the end goal towards which we take small steps. For the healthcare system, our super group collectively defined our vision as “providing a trustworthy and sustainable healthcare system that fosters collaborative and meaningful care for patients and staff in a society where everyone feels cared for.”
For any design project, we begin by establishing a vision based on what we would like the outcomes to look like, but we must really trust the process as it unfolds, recognizing that the vision may evolve along the way, and the steps taken towards achieving a vision are never going to be straightforward. When a government is reforming a system, a vision can be the guide that everyone follows, it motivates people to act. But, there could be a lot of challenges along the way, such as changes in political parties, challenges in administration, or lack of funding. A vision is what cuts across all the short-term challenges, to achieve the end goal. To build a trustworthy and sustainable healthcare system, it is not enough to have a system with continuity of care, it is only one of the steps to achieve the long-term vision. The challenges in the system are far bigger, there has been an erosion of the public healthcare system over time because of lack of funding, causing doctors to leave the public healthcare system due to stressful working conditions. Hence, to build a system where everyone feels cared for, the system needs fundamentally change to solve these issues.
Building the steps towards the vision
The Small Steps Matter
In the last few weeks, we have been brainstorming entry points that can help improve the healthcare system. 81% of health and social sector resources are consumed by only 10% of the population (Saltman & Teperi, 2016), and providing continuity to this 10% of the population will significantly reduce the load on the system. So we been exploring ways in which we can identify these heavy users and provide continuity of care to them while causing minimum changes to the existing system. What if there was a system where a patient visiting a doctor with certain conditions could be offered the choice to make further bookings with the same doctor for the entire course of the treatment? We called this “Continuity on Demand”, and this could provide continuity for the people when they need it the most. So, we explored the idea of creating an extension to Omakanta, where a doctor can approve, let’s say, 5 more appointments to the patient, and the patient can directly book the follow-up appointments on the app. Omakanta could also be improved to provide informational continuity, so patients feel that they have more transparency and control of their information. When we first thought of this idea, we really felt that we had the “aha” moment. Digitization of the existing system will make it more efficient, and having a centralized system for all the data can make life easier for everyone. As we started looking more into this solution, we started realizing that changing all the current data in the healthcare system to a digital system is not easy. In the past, many services, from booking appointments to mental health care appointments, have been digitalized without measures being put in place to mitigate the obstacles this poses for people with limited digital skills or without the financial means to buy suitable devices (“I Know I Won’t Get Help,” n.d.). Digitalization might not be the solution for our target user group, for example, elderly people who are heavy users of the system may not adapt to a digital platform easily. There are a lot of administrative challenges as well, and implementing an IT system comes with its own challenges in practice, like data and privacy concerns, legal concerns and challenges with the transition process.
Fear of the Unknown
How is policy made and implemented? As we have been working on this project, we have been realizing that there are two ways one could approach this. First, we can define our long-term vision and take bold steps to make big policy changes to reform the whole system in a short period of time. This policy, when unleashed, can shock the system for a while. Change is not comfortable, but people will adapt eventually. Our solutions can be small-scale changes that doesn’t change the existing system drastically. But this also means that the change towards our vision will not be achieved anytime soon. So, our approach needs to balance between bold large-scale changes to the system and making small interventions that can be piloted without changing the existing system. The middle ground would be to find solutions that are significant enough to nudge the system towards our vision to bring about large-scale change in the long run.

Discussions about entry points and solutions
Going Forward
We are currently exploring the idea of creating “Families of Care”, wherein healthcare centers are organized into teams comprising of doctors, nurses, and medical personnel who collaborate to oversee specific groups of patients. Through these care families, patients will benefit from consistent care, fostering trust, and everyone including medical staff could feel supported and cared for. We don’t know how our project will turn out eventually, and at this point, there are many opportunities and design interventions that we could explore, and all the opportunities pose their own unique challenges. The journey towards finding a solution continues, and we are constantly uncovering new breakthroughs, problems, and solutions, and in the process sharpening our understanding of how to implement positive change in the Finnish healthcare system.
References:
Saltman, R. B., & Teperi, J. (2016). Health reform in Finland: current proposals and unresolved challenges. Health Economics, Policy and Law, 11, 303–319. doi:10.1017/S1744133116000013
Amnesty International. (n.d.). “I Know I Won’t Get Help”: Inequality of healthcare in Finland.
The DfG course runs for 14 weeks each spring – the 2024 course has now started and runs from 26 Feb to 29 May. It’s an advanced studio course in which students work in multidisciplinary teams to address project briefs commissioned by governmental ministries in Finland. The course proceeds through the spring as a series of teaching modules in which various research and design methods are applied to address the project briefs. Blog posts are written by student groups, in which they share news, experiences and insights from within the course activities and their project development. More information here about the DfG 2024 project briefs. Hold the date for the public finale on Wednesday 29 May!