This blog post reports on work-in-progress within the DfG course! The post is written by group 2C dealing with the Ministry of Social Affairs and Health’s brief on Continuity of Care as a new Kela reimbursement.
The group includes Sofia Pascolo and Devayani Mohanraj from the master’s programme in Creative Sustainability, Heidi Mäkitalo from the master’s programme in Computer, Communication, and Information Sciences program (Human-Computer Interaction Major), and Robert Hartmann from the master’s programme in Collaborative and Industrial Design.
Written by: Sofia Pascolo
Imagine a world where your healthcare journey is smooth and continuous, where you’re not just another person on the list but a patient known and cared for by a dedicated team that understands your history and needs. This is the future of healthcare we envision – a future where your health is cared for proactively, continuously, and compassionately.
This world is not as far away from reality as you might think. But how do we reach it?
Let’s go back to where we left you with the last blog article. Since then, a lot has happened. We had just defined the vision of the three groups working on continuity of care and discussed our entry points in the ideations session. Now, we have a finalised design proposal that we presented in person at the Final Show.
We started by gathering insights from patients – the primary users of the system, which means all of us, including you. We interviewed people from various demographics, collecting stories and insights. One thing stood out from our research: the current system often makes you feel like a ping-pong ball, bouncing from one healthcare provider to another.
“The patient has a ping-pong role, going from one professional to another”
General Practitioner and Researcher
You’ve probably experienced this firsthand, telling your health history repeatedly. Or you might not because you rarely go to the doctor. We also observed these differences. We understood that different patients have different needs, priorities, and possibilities and that we needed to account for this complexity. Finland’s diverse healthcare providers – public, private, occupational, and student services – further complicate this fragmentation.
This dynamic also impacts health professionals in primary care, leaving them frustrated by the inability to witness the tangible outcomes of their treatments in patients, rather than merely addressing the symptoms of illness.
“It’s not health work, it’s sick work.”
General practitioner in a public primary healthcare
Ideating Solutions: From Fragmentation to Cohesion
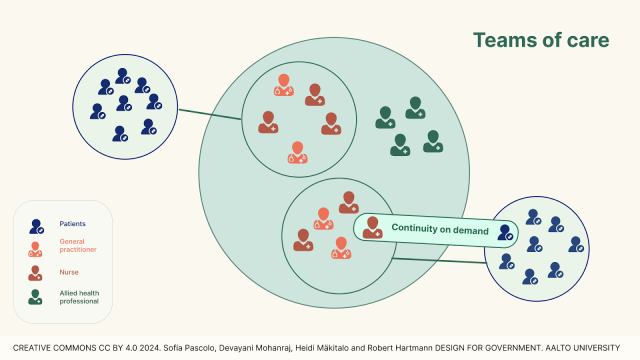
With these insights guiding us, we brainstormed ways to transform these fragmented experiences into a cohesive journey. Concepts like “family of care,” “continuity on demand,” and addressing the needs of “heavy users” started to take shape.
Imagine having a dedicated team of healthcare professionals who know your history and work together to provide continuous care. Imagine having the possibility to schedule follow-up appointments with doctors.
“The solution could be a personal team, consisting of 1-2 specialists and 1-2 trainee doctors, with whom nurses and the whole multi-professional team of social and health professionals would work. The team would take care of a specific group of patients and would get to know not only the patient but also each other,” reported the article “Continuity of care should not depend on a single doctor” (Helsingin Sanomat, 2022).
In addition to desk research, to ensure our ideas were practical and effective, we sought validation during the ideation session with the project partners and held workshops and interviews with general practitioners and health researchers. We’ve seen glimpses of this future in some health centres already, proving its feasibility on one side but also bringing us to reflect. Does it make sense to work on something that is already partially in place in some places?
Should we maybe find a way to exchange these best practices between different health centres? How can we bring them all to the same level? How can we streamline the transition of all health centres towards a system that supports continuity of care?
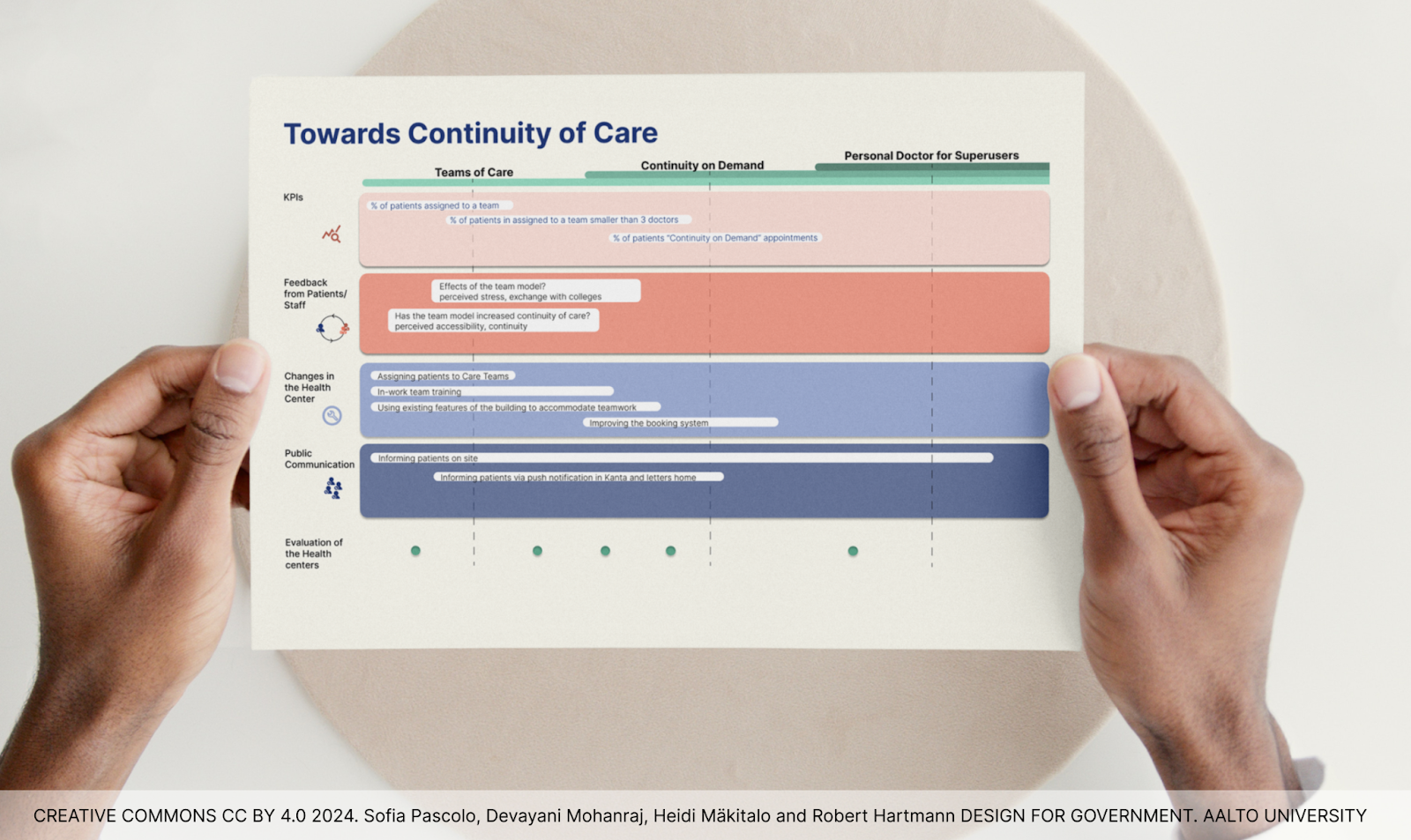
An adaptable and evolving action plan
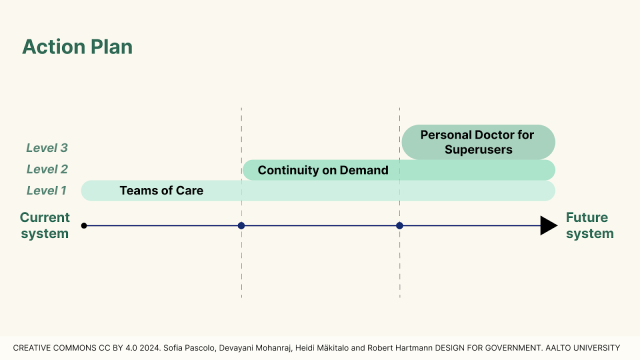
As our final proposal, we’ve developed an action plan to transition from the current system to one that ensures continuity of care. An action plan with 3 levels of continuity of care:
-
Teams of Care: a dedicated healthcare team responsible for you, consisting of doctors, nurses, and other professionals. This team approach means you’re more likely to see the same faces, fostering trust and better care.
-
Continuity on Demand: the possibility to decide together with a nurse and/or general practitioner the necessity to schedule follow-up appointments to monitor your progress.
-
Personal Doctors for “superusers”: some of us need more continuity than others, think about chronically ill or elderly patients. This system allows the assignment of personal doctors to these “superusers” and can provide them with consistent, focused care, easing the strain on the healthcare system and improving their outcomes.
The levels have different interventions to help to move forward. Through these interventions each health center will have the flexibility to evolve at its own pace but within a shared framework and towards a common goal.
Detailed descriptions of each level and the associated interventions will be available in our final document, which will be published on the Design for Government website. Be sure to review it!
In conclusion, our adaptable and evolving action plan signifies a major shift from the current “sick care” model, where patients seek care reactively, to a proactive healthcare system. Here, patients are not merely customers but integral members of a dedicated healthcare team, receiving continuous and comprehensive care.
This transformative approach promises to elevate both the healthcare system’s effectiveness and the patient experience, leading to improved outcomes. By addressing the root causes of fragmentation and promoting proactive care, our proposal lays the groundwork for a more cohesive and patient-centred healthcare system.
Human-centric approaches emerged as a common thread at the Final Show of the Design for Government Course where we had the opportunity to share our proposal with stakeholders, project partners, and fellow students. Among the six groups and two challenges addressed, “Continuity of care” and “Policy Coherence for Biodiversity,” we observed a shared focus on people, relationships, interactions, and feelings. This emphasis underscores the significance of leveraging design thinking methods – system thinking, strategic design, and behavioural-based design – in policymaking for complex societal issues.
References:
Braam, A., Buljac-Samardzic, M., Hilders, C. G., & van Wijngaarden, J. D. (2022). Collaboration Between Physicians from Different Medical Specialties in Hospital Settings: A Systematic Review. Journal of Multidisciplinary Healthcare, Volume 15, 2277–2300. https://doi.org/10.2147/jmdh.s376927
Continuity of care in primary care 2022. (2023). THL. file:///Users/sofiapascolo/Downloads/Hoidon%20jatkuvuus%20perusterveydenhuollossa_Tilastoraportti_TV2022_final_saavutettava.pdf
Continuity of care should not depend on a single doctor. (2022, April 13). Helsingin Sanomat. https://www.hs.fi/mielipide/art-2000008744359.html
General practitioner and researcher at Tampere University. (2024).
General practitioner in public primary healthcare. (2024).
Ideation session – Design for Government course. (2024, May 8).
Is health insurance really for health care? (2016, November 8). Pittsburgh Upper Cervical Chiropractic. https://pittsburghuppercervical.com/sick-care-vs-health-care/
Masterson, K. (2014, August 26). A Team-Based Approach to Primary Care. A Team-Based Approach to Primary Care | UC San Francisco. https://www.ucsf.edu/news/2014/08/116856/team-based-approach-primary-care
The DfG course runs for 14 weeks each spring – the 2024 course has now started and runs from 26 Feb to 29 May. It’s an advanced studio course in which students work in multidisciplinary teams to address project briefs commissioned by governmental ministries in Finland. The course proceeds through the spring as a series of teaching modules in which various research and design methods are applied to address the project briefs. Blog posts are written by student groups, in which they share news, experiences and insights from within the course activities and their project development. More information here about the DfG 2024 project briefs.