This blog post is a progress report on our work for the DFG course 2024. It’s written by Atte Kuparinen, a member of Group 2A. It focuses on the brief provided by Kela and the Ministry of Social Affairs and Health regarding continuity of care. Our group 2A consists of Atte Kuparinen and Emma Prost from collaborative and industrial design and Beste Polatkal and Thekla Weißkopf from the Creative Sustainability Design program.
Written by: Atte Kuparinen
A Recap of Our Latest Accomplishments
Dear reader, as you might know from the earlier blog post, our team, 2A, has researched public healthcare administration to identify potential risks to continuity of care in the present or near future.
During this research phase, we have gained an understanding of the working environment of a general practitioner (GP), as well as the administrative structure that supports their regular work. We also recognized the potential risks of a shortage of GPs in public healthcare that may arise in the coming years.
We focused the research on identifying the causes of the emerging shortage of doctors and the limitations of their education and hiring. We found very limited ways to prevent this GP shortage. In this very moment, the best course of action, in our opinion, is to ensure that GPs’ current work won’t run off and their valuable working time is used efficiently. To determine how to achieve that, we analyzed the healthcare administration structures, considering the viewpoints of GPs operating in both the public and private sectors. We aimed to identify the primary stakeholders who could provide support to GPs and enhance their work experience.
We conducted interviews with four doctors: one medical director, one from the public primary sector, one from the public specialized sector, and one from the private sector. The interviews aimed to gain insights into their weekly tasks, experiences, and challenges and identify opportunities to improve their workflow. All the doctors we interviewed expressed that they are burdened with an excessive amount of administrative paperwork that is not related to their specialization. Two of these doctors pointed out that they would need help with paperwork and booking, to make the work more efficient and desirable, and that there is an overall lack of secretaries working in the public healthcare sector. We also discovered that many GPs find working in the public sector overwhelming compared to the rewards they receive, leading them to seek more comfortable better-paid work in the private sector.
After discovering these findings, we are now working to enhance the dynamics of primary healthcare teams regarding patient work. We need to find answers to questions like:
1. How to reduce and streamline the administrative work of doctors and nurses?
2. What physical and confidentiality barriers does the medical team need to address in their work?
3. How is information typically shared in the public healthcare system?
4. How can the trust within a medical team be improved and strengthened?
To find answers to these questions and to create an optimal medical team structure, we have planned a collaborative workshop for a doctor, nurse, and secretary in the upcoming weeks.
How to Create a Shared Vision and Find a Good Entry Point
Last week, the whole healthcare team was given the task of coming up with a vision that all three healthcare teams (2A, 2B, 2C) could stand behind. Why is this important, and why is it crucial to have a vision?
So far, our team has not established a common, clear vision of the outcomes we aim to achieve through this project. We assumed that our team shares similar values in life, but this has been only an assumption. When discussing topics such as reducing services or utilizing natural resources, it becomes evident that clarifying our vision and developing a common understanding is crucial to building a strong team.
“Leverage Points” by Donella Meadows (1999) highlights the importance of having a vision or mindset. Meadows emphasizes that the mindset or paradigm from which a system arises is a crucial leverage point. She mentions Jay Forrester’s idea that the shared beliefs and assumptions within a society, which constitute its paradigm, greatly influence how the system operates (Meadows, 1999).
It was a challenge to find a common vision or leverage point for all the healthcare groups, as their research areas were different. We wanted the vision to be both inspirational and ambitious, but also tangible and realistic. After quick consideration, we arrived at a powerful and hopeful message that we all agreed would be worth working towards:
“We provide a trustworthy and sustainable healthcare system that fosters collaborative and meaningful care for patients and staff in a society where everyone feels cared.”
The vision presented appears to align with the assumptions we have made in this course and project, and with those of our peer students. However, it is important to note that the vision is quite idealistic and lacks depth. It does not address any radical changes that could be made to the system. If the goal of the project is to bring about radical change, the vision must clearly reflect this. Therefore, having a clearly defined shared vision is crucial for the success of any project.
Seeking the entry point.
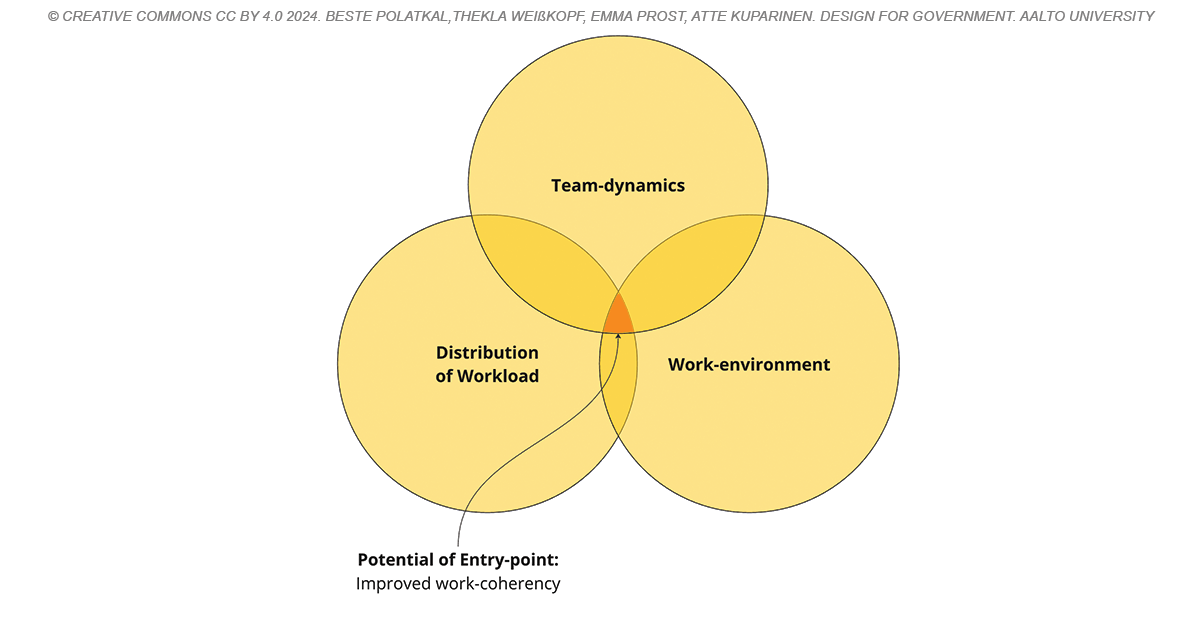
A clear common vision should include the desired leverage point of the project. We are defining possible entry points for our draft proposal of improved team dynamics in primary healthcare.
What would be the most efficient way to start improving team dynamics? There are an endless amount of factors that contribute to healthy team dynamics, but what would be a realistic number of variables to focus on without overwhelming the team?
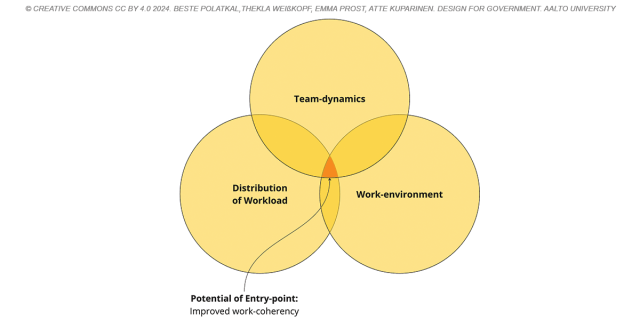
This is still a work in progress, but we believe that by improving the mental aspect of team dynamics, workload distribution, and working environment, we can enhance conditions not only for GPs but for everyone involved in the public healthcare system.
After our workshop with the multi-disciplinary healthcare team, we aim to have a clear team vision and optimized entry point to leverage the change in public healthcare workforce shortages. We may have even some strategies to propose that can attract GPs back to the public sector. To find out what occurred, please read our upcoming blog post.
References:
1. Meadows, D. (1999). Leverage Points: Places to Intervene in a System. Hartland: The Sustainability Institute.
The DfG course runs for 14 weeks each spring – the 2024 course has now started and runs from 26 Feb to 29 May. It’s an advanced studio course in which students work in multidisciplinary teams to address project briefs commissioned by governmental ministries in Finland. The course proceeds through the spring as a series of teaching modules in which various research and design methods are applied to address the project briefs. Blog posts are written by student groups, in which they share news, experiences and insights from within the course activities and their project development—more information here about the DfG 2024 project briefs. Hold the date for the public finale on Wednesday 29 May!