This blog post reports on work-in-progress within the DfG course! The post is written by Beste Polatkal, a member of group 2A. Together, we work in collaboration with the KELA and Ministry of Social Affairs & Health’s brief on ‘Towards a Better Healthcare System: Exploring Continuity of Care’. Group 2A includes Atte Kuparinen and Emma Prost from the Collaborative & Industrial Design program, Beste Polatkal, and Thekla Weißkopf from the Creative Sustainability – Design program.
Written by: Beste Polatkal
As a team diving into our initial research, we’ve chosen to focus on identifying the key problem areas within Finnish healthcare system. Why? Because pinpointing these trouble spots gives us a clearer entry point to discover potential opportunities for improvement from an administrative angle. We believe that tackling these issues from this point can not only bring about meaningful improvements but also trigger significant, system-wide changes. According to Donella Meadows (1999) these changes often start from what are called ‘leverage points’—strategic spots in a complex system where a small tweak can have large, far-reaching effects.
But here’s the thing: understanding these complex systems and pinpointing the exact leverage points requires a comprehensive, all-angles approach. That’s why we’ve been deep-diving into both desk research and interactive interviews and workshops. We’ve committed to mapping out how these problems interconnect and digging down to their root causes, which is crucial for truly understanding how to make impactful changes. Using the ‘5 Whys’ technique, we’ve started peeling back the layers of each issue for our midterm presentations. Let me take you through some of the critical ‘Why?’ questions we’ve tackled.
Threat of Discontinuity & Unmet Demand
Let’s talk about the discontinuity of care—a pressing issue here in Finland that our brief has highlighted. Our first “Why?” led us to the initial insight that there simply aren’t enough doctors. Therefore, the trend in doctor numbers is not increasing. This was something we felt intuitively from our interviews, but when we looked at the numbers from Lääkäriliitto’s 2019 report, we were surprised. It turns out the number of doctors has been on the rise, thanks to recent reforms.
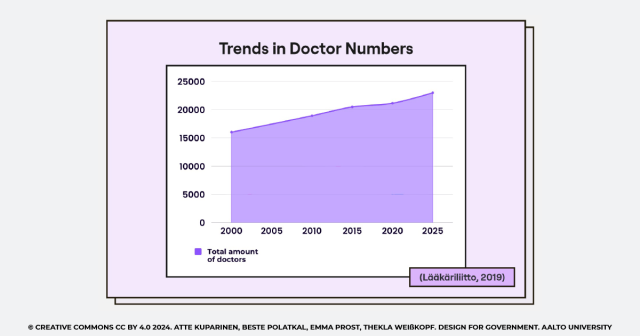
Fig 2. – Trends in Doctor Numbers
But here’s the catch—despite these efforts, there’s still an evident unmet need and doctor shortage. Long patient queues are a common sight, and with Finland’s demographics rapidly changing, just increasing the number of medical students isn’t going to cut it. The real challenge lies deeper—it’s about the value. This is how we navigated to our second ”Why?” question.
Workload and Work Conditions
Why is there still an unmet demand in Finnish healthcare? Our research points to the workload and working conditions as the causes. The current setup demands so much from healthcare workers that it becomes counterproductive. Think about it: doctors spend around 8 hours a week just on paperwork, according to STM (2022). That’s a whole workday gone to administrative tasks each week!
This intense workload creates a working environment that is not just inefficient but also isolates healthcare professionals from their peers and patients—essentially, an asocial environment. It’s not just about the long hours; it’s about the nature of the work they’re doing, including a load of non-medical tasks. So, this leads us to another pressing question: Why is the workload so demanding?
Doctor Attrition
The demanding nature of the job has been driving doctors away. Many physicians are either leaving the public sector altogether or cutting back their hours. And here’s another catch: as more doctors leave or reduce their hours, the workload for those who remain becomes even more demanding.
This chain relationship continually spirals, creating more reasons for medical staff to feel overwhelmed and underappreciated. Each departure puts additional strain on the remaining staff, extending a cycle of burnout and attrition. This deep dive into the core issues reveals a vicious cycle, one that underscores the urgent need for better working conditions and teamwork to reduce excessively demanding workloads.
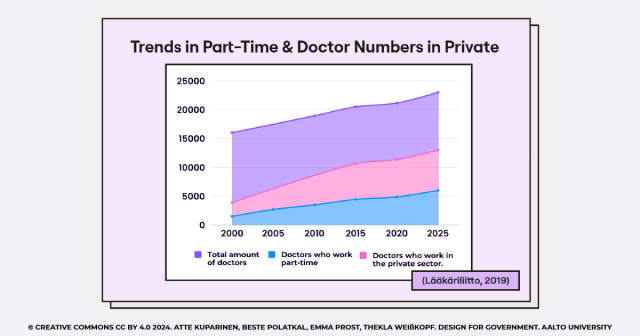
Fig 3. – Trends in Part-Time & Doctor Numbers in Private
Opportunities: Teamwork
Our research strongly supports the implementation of team-based care as a transformative strategy for healthcare settings. According to a recent study by Porter et al. (2022), adopting this model has been shown to reduce the time physicians spend on direct patient care by one-third, significantly enhancing operational efficiency and increasing patient capacity. This finding highlights the potential of collaborative care models not just to improve outcomes but also to optimize healthcare delivery.
Furthermore, our interviews have uncovered a critical gap in the Finnish healthcare system—the overwhelming burden of administrative tasks on doctors. This insight highlights the urgent need for more secretarial support, pointing to an invaluable opportunity to enhance care delivery by reducing the administrative load on medical professionals. Addressing this from an administrative perspective could greatly improve efficiency, continuity, and job satisfaction for medical staff through empowering teamwork.
Looking Forward
As we continue our journey to explore continuity in healthcare in Finland, we are reminded of the power of collaborative effort—not just in healthcare settings but within our own team. For our midterm presentation, we worked hard collaboratively and challenged ourselves to present our research without the usual slide deck. Instead, we compiled a comprehensive handout summarizing our findings & identified opportunity areas, and divided the work according to our strengths. This teamwork and collaboration made me believe that -by leveraging each other’s strengths, we can overcome complex challenges. So far it has been a pleasure for me to work with my team on this project, I am looking forward to going further to explore continuity in Finnish Healthcare!

Fig 4. – Midterm Presentation
REFERENCES
Lääkäriliitto. (2019). Physicians Report. https://www.laakariliitto.fi/site/assets/files/5256/sll_taskutilasto_en_220620.pdf
Meadows, D. (1999). Leverage Points: Places to Intervene in a System. Hartland: The Sustainability Institute.
Porter, J., Boyd, C., Skandari, M.R. et al. Revisiting the Time Needed to Provide Adult Primary Care. J GEN INTERN MED 38, 147–155 (2023). https://doi.org/10.1007/s11606-022-07707-x
STM. (2022). Omalääkäri 2.0 -selvityksen loppuraportti. https://urn.fi/URN:ISBN:978-952-00-9884-1
The DfG course runs for 14 weeks each spring – the 2024 course has now started and runs from 26 Feb to 29 May. It’s an advanced studio course in which students work in multidisciplinary teams to address project briefs commissioned by governmental ministries in Finland. The course proceeds through the spring as a series of teaching modules in which various research and design methods are applied to address the project briefs. Blog posts are written by student groups, in which they share news, experiences and insights from within the course activities and their project development. More information here about the DfG 2024 project briefs. Hold the date for the public finale on Wednesday 29 May!