This blog post reports on work-in-progress within the DfG course! The post is written by group Care 1 dealing with Kela, the Social Insurance Institution of Finland’s brief on “Continuity of Knowledge” in healthcare. The group includes Francesca Martini from Creative Sustainability program (Aalto University), Paola Rapino from Creative Sustainability (Aalto University, Exchange), Huang Tzu-Tai from Sustainable Entrepreneurship (Aalto University), and Joni Lappalainen and Takashige Doi from the Collaborative and Industrial Design program (Aalto University).
Written by: Joni Lappalainen
As we know, the human nervous system is a remarkable web of interconnected pathways, constantly transmitting information to maintain coordination. Just as neurons communicate seamlessly to ensure the body functions optimally, healthcare systems must achieve a similar continuity of knowledge to provide effective and continuous patient care. However, fragmentation in continuity of knowledge can lead to gaps in knowledge, miscommunication, and inefficiencies in treatment in the healthcare system.
But how can a fragmented healthcare system, spread across multiple providers and information sources, maintain continuity of knowledge between organizations while safeguarding patient care?
This year, one of the two challenges that the Design for Government course builds upon is the theme of Continuity of Care. The project is a collaboration with Kela, the Social Insurance Institution of Finland, focusing on how healthcare services can build and maintain a continuity of knowledge.
“A quarter of the Finnish population will be over 65 by 2030”
The increasing demographic trend, with projections indicating that a quarter of the Finnish population will be over 65 by 2030, is expected to place significant pressure on the care system (Ministry of Social Affairs and Health, 2020). Integrating patient-centered services into the care system requires encompassing preventative healthcare to mitigate potential system overload, which will affect even me and you (Tynkkynen, et. Al., 2022).
What is Continuity of Knowledge in Healthcare?
In our project, our group sees Continuity of Knowledge as more than just raw data in healthcare. Continuity of Knowledge is about ensuring that the correct information, whether related to medical, social, or personal care, isn’t just stored, but actively communicated and transformed into helpful understanding. It’s about ensuring that knowledge doesn’t vanish within the system, but instead, contributes to better care and decision-making for patients (Moilanen, et al. 2025).
We have identified four essential aspects Continuity of Knowledge:
- Sustained knowledge transfer. Information needs to flow smoothly between all stakeholders, without unnecessary barriers.
- Information emerges from lived experiences. Data isn’t enough on its own; it needs to be related to a real-world context of patient care.
- Bridging quantitative and qualitative data. Statistics are important, but they have to be balanced with human experiences to create a complete picture.
- Strengthening collaboration. Care professionals from different fields and patients should work together, ensuring that care decisions are meaningful.
As our group sees it, continuity of knowledge is a crucial aspect of healthcare, particularly as Finland faces a growing demand for elderly care.
Fragmentation of Knowledge in the Healthcare System
Our group believes that fragmentation happens between different healthcare system levels (see figure 1). The care system could be viewed through medical care, social care, and informal care.
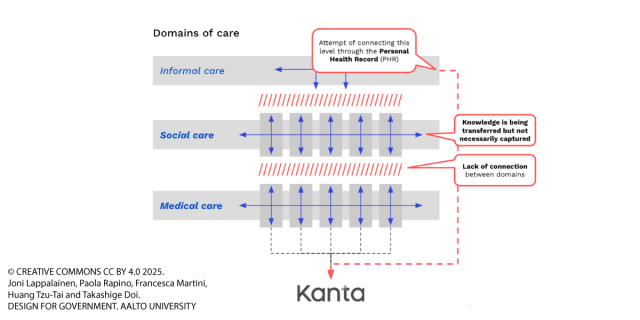
Figure 1 Different levels of care domains.
As illustrated (figure 1), medical care features structured data from different providers in Kanta. Meanwhile, social care data is partly integrated but often lacks connection to medical care, and informal care data tends to be fragmented or unrecorded. An ongoing attempt is to connect these different levels of care through the Personal Health Record (PHR) (Yliruka, et al., 2024.).
Our figure highlights the challenges in achieving a comprehensive view of an individual’s care needs across these domains. We believe this knowledge is not always effectively captured, and there is a lack of connection between the different care domains.
The Crucial Role of Social Workers within the System
Social workers are crucial in transferring experience-based knowledge within healthcare and social care systems (Kettunen & Enroos, 2023). Our group trusts that social workers bridge the gap between patients, families, and formal care providers, allowing for a more seamless flow of knowledge and ensuring that critical insights are not lost during patient-care transitions.
“Social workers are crucial in transferring experience-based knowledge within healthcare”
By engaging with individual patients, social workers can capture and transfer knowledge that may not be documented in formal records — such as patient’s emotional well-being, personal preferences, and informal care arrangements. This knowledge is essential in maintaining continuity of care and improving patient outcomes.
However, to our knowledge, recognizing the added value of human interaction in knowledge continuity remains a challenge. How can we ensure that social workers’ insights are effectively integrated into care practices?
Learning from the Field: Understanding Social Workers
To gain deeper insights of social workers, our team will be conducting fieldwork through observations and interviews. By visiting elderly care facilities and observing social workers in their daily interactions with patients, we aim to understand the nuances of their work. For insightful research, we need to know how they gather, communicate, and apply knowledge that may not be formally recorded.
We believe these firsthand experiences will help us identify opportunities for the next step, ensuring that their valuable contributions lead to better, more connected patient care in Finland.
References
Kettunen, P., & Enroos, R. (2023). Health social workers and research knowledge utilisation. European Journal of Social Work, 1–12.
Ministry of Social Affairs and Health. (2020). Quality recommendation to guarantee a good quality of life and improved services for older persons 2020–2023.
Moilanen, E., Ojajärvi, A. & Rosenlund, M. (2025, March 11). Roundtable discussion. Aalto University.
Tynkkynen, L.-K., et. al. (2022). Health system reforms and the needs of the ageing population—An analysis of recent policy paths and reform trends in Finland and Sweden.
Yliruka, L., Heino, E., & Pohjola, V. (2024). Perceived effects of digitalization on social work in Finland: Opportunities and challenges in practice. International Social Work.
The DfG course runs for 14 weeks each spring – the 2025 course has now started and runs from 24th Feb to 27th May. It’s an advanced studio course in which students work in multidisciplinary teams to address project briefs commissioned by governmental ministries in Finland. The course proceeds through the spring as a series of teaching modules in which various research and design methods are applied to address the project briefs. Blog posts are written by student groups, in which they share news, experiences and insights from within the course activities and their project development. More information here about the DfG 2025 project briefs. Hold the date for the public finale on Tuesday 27th May!